
Expert Care for Skin Cancer Diagnosis and Treatment
Types of skin cancer we treat
At Advanced Dermatology, P.C., we offer state-of-the-art, minimally invasive interventions that treat the following forms of skin cancer:
Basal Cell Carcinoma
Basal cell carcinoma is the most common form of skin cancer, accounting for about 80% of all cases according to Yale Medicine. It originates in the basal cells, which are found in the deepest layer of the epidermis.
Basal cell carcinoma is a highly treatable form of cancer that is only rarely life-threatening. Symptoms include the following:
- Flat, flesh-colored or brown lesions
- Bleeding sores that won’t heal
- Scaly, red splotches
- Small, translucent, shiny nodules
- Crusty or oozing areas
- Itchy or tender spots
- Skin growths with raised edges and a central indentation
- Growths with visible blood vessels

These symptoms can appear on sun-exposed areas like the face, ears, and neck. While prolonged sun exposure is the most common predictor of basal cell carcinoma, other risk factors include family history of skin cancer, radiation exposure, arsenic exposure, and a compromised immune response.
Treatment options include surgical excision, curettage and electrodesiccation, cryotherapy, and Mohs micrographic surgery. Early detection and treatment are crucial for successful outcomes.
Squamous Cell Carcinoma
Squamous cell carcinoma is the second most common form of skin cancer, arising from the flat, scale-like squamous cells that make up the outermost layers of the epidermis.
While anyone can get squamous cell carcinoma, people with fair skin, light hair, and light eyes are at a higher risk. It is often caused by prolonged or intense exposure to ultraviolet (UV) radiation from the sun or tanning beds, and typically develops on sun-exposed areas like the face, ears, neck, and hands.
Though squamous cell carcinoma is generally highly treatable and slow-growing when caught early, it can become life-threatening if left untreated. In advanced stages, it can grow deep into the skin, causing local tissue damage and potentially spreading to the lymph nodes and other parts of the body, which can be fatal.
Recognizing the signs of squamous cell carcinoma is vital for early detection and successful treatment. Symptoms can vary, but generally include changes to the skin that may be visible or felt. Common symptoms include the following:
- A hard, red bump or nodule.
- A flat lesion with a scaly or crusted surface.
- A new sore or a raised area on an old scar or sore.
- An open sore that doesn’t heal, or that heals and then reappears.
- A rough, scaly patch on the lip that may turn into an open sore.
- A rough or scaly red (or darker) patch that might crust or bleed.
- A wart-like growth.
- A sore or rough patch inside the mouth.
- A raised, wart-like sore on or in the anus or on the genitals.
Cutaneous T-Cell Lymphoma
Cutaneous T-cell lymphoma (CTCL) is a rare form of non-Hodgkin lymphoma that develops in the skin from T-lymphocytes, which are white blood cells that normally fight infection. The exact cause is unknown, but it occurs when these T-cells become abnormal, grow out of control, and migrate to the skin.
Common symptoms include dry, red, and scaly patches, plaques, or skin tumors. In more advanced cases, it can spread to the blood, lymph nodes, and other organs. Risk factors may include older age, being male, and having a compromised immune system.
While often slow-growing and manageable, CTCL can be dangerous if it progresses and spreads beyond the skin. Potential dangers include the following complications:
- Systemic disease
- Increased risk of skin infections
- Swollen lymph nodes
- Hair loss
Treatments vary depending on the stage and can include skin-directed therapies like topical corticosteroids, topical chemotherapy, and radiation therapy, or systemic treatments such as oral medications, chemotherapy, or photopheresis, which removes and treats blood with UV light.
Melanoma (Adult)
Melanoma originates in melanocytes, the cells in the skin that produce melanin and determine skin color.
The most significant danger of this serious form of skin cancer is its aggressive nature and propensity to metastasize, or spread quickly, to other parts of the body. If left unaddressed, melanoma can invade deep into the skin and reach the bloodstream or lymphatic system, potentially spreading to vital organs like the liver, brain, bones, and lungs.
While commonly developing on sun-exposed areas of the skin, melanoma can also appear in less obvious places that receive little to no sun. Hidden areas where melanoma might develop include the following:
- Under the nails
- Palms of the hands
- Soles of the feet
- Eyes
- Mucous membranes
Potential warning signs include the following symptoms:
- A mole that looks significantly different from other moles on your skin.
- A mole that itches, bleeds, or becomes tender or painful.
- A new bump or nodule, which may be red, pink, flesh-colored, or colorless in the case of amelanotic melanoma.
- A dark streak under a fingernail or toenail.
- A dark spot on the iris or a change in vision in the case of ocular melanoma.
- Dark spots or irregular areas on the palms, soles, or in mucous membranes.
The success of treatment is highly dependent on early detection, as melanoma is largely curable when diagnosed at its earliest stages before it has the chance to spread. However, the outlook is significantly worse once it has metastasized to distant parts of the body.

Melanoma in Children
Pediatric melanomas develop from melanocytes, the cells responsible for producing pigment in the skin, when their DNA changes and causes them to grow uncontrollably.
Intense sun exposure leading to sunburns is a known risk factor, particularly in fair-skinned individuals. However, it is not the sole cause; some childhood melanomas, especially those in very young children, are not strongly linked to UV light. Common risk factors include the following:
- Having a family history of melanoma.
- Multiple moles or large congenital nevi (birthmarks).
- Compromised immune system health.
Melanoma in children is often different from adult melanoma, which can make it challenging to diagnose. The primary danger of childhood melanoma is its potential to metastasize, or spread to other parts of the body.
According to statistics from the Melanoma Research Foundation, melanoma is the deadliest form of skin cancer. Nevertheless, when caught early, the prognosis is usually excellent, with early-stage cases being highly curable, but late detection significantly worsens the outcome.
Treatment options typically include surgical removal of the tumor and a margin of healthy tissue, and for more advanced cases, a combination of other therapies like immunotherapy, targeted therapy, and chemotherapy.
Symptoms of melanoma in children include the following:
Unexplained fatigue, weight loss, chronic cough, or headaches, which could indicate the cancer has spread.
- A new bump on the skin that bleeds, crusts, or itches.
- A new or changing mole that may not be dark in color, appearing instead as pink, reddish, yellowish, or whitish.
- A wart-like, non-pigmented spot.
- An odd-looking or fast-growing mole.
- A mole that looks significantly different from a child’s other moles.
- Unexplained fatigue, weight loss, chronic cough, or headaches, which could indicate the cancer has spread.
FAQs about skin cancer
Learn more about skin cancer: your risk, the signs, and how it can be prevented.
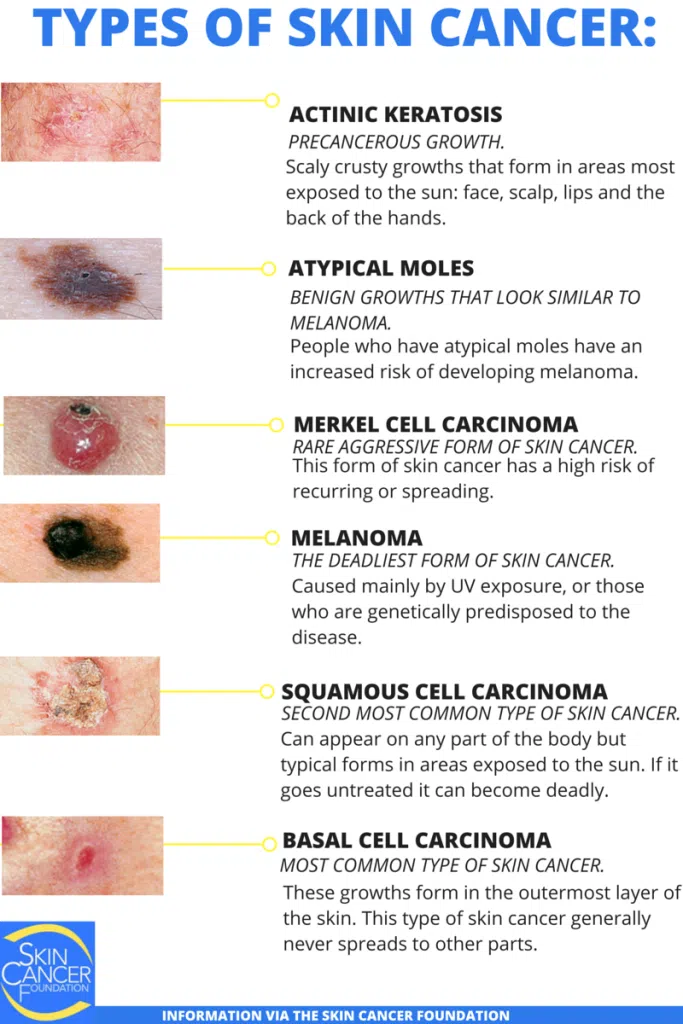
What are the main types of skin cancer?
The most prevalent forms of skin cancer include the following:
Squamous Cell Carcinoma
Squamous cell carcinoma is the second most common type of skin cancer, often linked to prolonged UV exposure. It typically develops on sun-exposed areas such as the face, ears, and hands, and can sometimes spread to other parts of the body.
- Symptoms include scaly, red patches, open sores, or wart-like growths that may crust or bleed.
- Early detection is crucial, as SCC can become aggressive and spread to lymph nodes.
- Treatment options include surgical removal, cryotherapy, or radiation therapy, depending on the severity.
Basal Cell Carcinoma
Basal cell carcinoma is the most common form of skin cancer, often caused by cumulative sun exposure. It usually appears on areas like the face and neck and rarely spreads to other parts of the body, though it can cause significant local damage if untreated.
- Symptoms include shiny, raised pimple-like bumps, flat, flesh-colored or dark lesions, and sores that bleed or don’t heal.
- Basal cell carcinoma grows slowly and is highly treatable when detected early.
- Treatment often involves surgical excision, curettage, or topical medications.
Melanoma
Melanoma is the most dangerous type of skin cancer, originating in the pigment-producing cells (melanocytes). It can develop anywhere on the body, including areas not exposed to the sun, and has a higher risk of spreading to other organs.
- Symptoms include moles with irregular borders, asymmetry, color variations, or changes in size and shape.
- Early detection is critical, as melanoma can be life-threatening if untreated.
- Treatment typically involves surgical removal, and advanced cases may require chemotherapy or immunotherapy.
What does skin cancer look like?
Potential skin cancer signs include the following:
- Any mole that stands out from the others: Look for different sizes, shapes, or colors.
- Non-healing sores: A sore or lesion that bleeds, oozes, or crusts over and doesn’t heal within a few weeks should be evaluated.
- New or changing growths: Any new bump, patch, or mole, or a change in an existing one, can be a sign of skin cancer.
- Wart-like growths: A bump that resembles a wart can sometimes be skin cancer.
- Itching or pain: While not always present, some skin cancers can cause new or changing sensations like itching, tenderness, or pain.
- Scar-like patches: Basal cell carcinoma can sometimes appear as a flat, firm, pale, or yellow area resembling a scar.
- Persistent red patches: A rough, scaly, red patch that may crust or bleed is a common sign of squamous cell carcinoma.
It is highly recommended to perform regular at-home skin checks to become familiar with your skin and spot any changes early. However, self-exams are not a substitute for professional evaluation.
A board-certified dermatologist should conduct periodic, full-body skin checks, especially for those with risk factors like excessive sun exposure, a personal or family history of skin cancer, or numerous or atypical moles. Early detection by a professional significantly increases the likelihood of a successful and less invasive treatment.
How is skin cancer diagnosed?
Skin cancer is typically diagnosed through a combination of visual skin exams and biopsies. During a visual exam, a physician inspects the skin for unusual growths or changes in moles, while a biopsy involves removing a small sample of tissue for closer examination under a microscope.
In some cases, laboratory analysis is performed to confirm the presence of cancer and identify its type. If skin cancer is confirmed, additional tests such as imaging or lymph node biopsies may be recommended to determine if the cancer has spread, a process known as cancer staging.
What treatments are available for skin cancer?
Several treatment options are available for skin cancer, depending on the type and severity, including the following interventions:
- Topical treatments: Non-life-threatening, superficial forms of skin cancer might be effectively treated with topical medications.
- Cryosurgery: Treatment involving freezing the lesion using liquid nitrogen.
- Cancer excision: Surgical removal of cancerous tissue.
- Mohs micrographic surgery: A tissue-preserving surgical technique.
Can skin cancer be prevented?
Your risk of skin cancer can be dramatically reduced by following several key strategies. The Centers for Disease Control and Prevention (CDC) recommend avoiding excessive sun exposure, using broad-spectrum sunscreen with at least SPF 30, wearing protective clothing, and seeking shade during peak sun hours.
Moreover, avoid tanning beds and sun lamps, which are mechanisms for delivering ultraviolet light at a greater intensity than the sun, according to the National Center for Health Research.
Regular skin checks by a board-certified dermatologist are also essential for early detection and prevention. These periodic exams can help identify any unusual changes or growths, allowing for timely intervention and reducing the risk of skin cancer development.
